Introduction to Emergency Care Systems
Summary
Effective emergency care systems rely on clarity around terms, rights, and responsibilities. Globally inconsistent definitions hinder advocacy, coordination, and resource allocation. The WHO Framework and World Health Assembly resolutions now position emergency care as essential to resilient health systems. Addressing key evidence gaps and foundational questions about impact and priority-setting will guide effective global health improvements in emergency care.
Why Define Emergency Care Systems?
Emergency physicians are trained to think in moments: identifying threats, stabilizing patients, making decisions under uncertainty. But our work also sits inside—and is often constrained by—a broader system. That system determines whether a patient reaches us in time, whether we have the resources to intervene, and what happens to them afterward.
Despite the central role emergency care plays in saving lives, it’s often overlooked in health systems planning. Part of the problem is semantic. “Emergency care” is used inconsistently across disciplines and countries. “Emergency medicine,” “acute care,” and “prehospital care” are frequently conflated. Without clarity, it’s hard to build systems that are intentional, responsive, and equitable.
By establishing shared definitions and frameworks, we not only improve communication between clinicians, policymakers, and funders—we also equip ourselves to better advocate for systems that work.
What Is Emergency Medicine?
Emergency medicine (EM) is a relatively new specialty, especially in global terms. While it’s well established in some countries, many health systems are only just beginning to formally train EM physicians or integrate EM services.
Here are three widely used definitions:
- American College of Emergency Physicians (ACEP): EM is “the medical specialty dedicated to the diagnosis and treatment of unforeseen illness or injury.”
- Australasian College for Emergency Medicine (ACEM): It is “a medical specialty that equips doctors with the knowledge and skills required to care for people with life threatening or urgent health care needs.”
- International Federation for Emergency Medicine (IFEM): EM is “a field of practice based on the knowledge and skills required for the prevention, diagnosis, and management of acute and urgent aspects of illness and injury... It further encompasses an understanding of the development of prehospital and in-hospital emergency medical systems and the skills necessary for this development.”
What’s notable is how all three definitions emphasize unpredictability, acuity, and breadth—but IFEM goes further, embedding system-level thinking into the core of the specialty. This framing positions emergency medicine not just as clinical work, but as a systems-oriented discipline.
What Is Emergency Care?
If emergency medicine is the specialty, emergency care is the function. It spans disciplines and settings. A bystander providing CPR, a health worker giving oxytocin in a rural clinic, and a physician managing polytrauma are all delivering emergency care.
The Disease Control Priorities Project (DCP3) offers one of the most practical definitions:
"Emergency care includes health services for conditions that require rapid intervention to avert death or disability, or for which delays of hours can worsen prognosis or reduce effectiveness."
This definition captures several key ideas:
- Timeliness is critical.
- Outcomes—not settings—define urgency.
- Perception matters: even self-identified emergencies deserve response.
This framing helps shift emergency care from being seen as a luxury of well-resourced hospitals to a core, essential health service that must be available wherever people live.
Emergency Care in Global Health Policy
Emergency care has historically been underrepresented in global health initiatives, which often focus on vertical programs like immunization, HIV, or maternal health. That’s changing.
Three major World Health Assembly (WHA) resolutions have helped formalize the role of emergency care in global health:
- WHA 60.22 (2007): The first resolution calling on countries to strengthen emergency care systems as part of broader health systems strengthening.
- WHA 68.15 (2015): Positioned emergency care as an essential component of universal health coverage (UHC).
- WHA 72.16 (2019): Endorsed the WHO Emergency Care Systems Framework and highlighted emergency care as key to health system resilience and SDG implementation.
These resolutions provide political leverage. They give clinicians and advocates a basis for pushing national governments and donors to prioritize emergency care in planning and funding.
Constitutional Rights and Legal Foundations
Access to emergency care is increasingly recognized as a human right. A legal review of 195 national constitutions found that ten included explicit provisions for emergency care. These go beyond aspiration—they often outline enforceable rights and responsibilities. Examples include:
- Somalia (2012): “No one may be denied emergency healthcare for any reason, including lack of economic capability.”
- Ecuador (2008): “Public or private institutions... shall not refuse emergency care. This refusal shall be punishable by law.”
- Fiji (2013): “A person must not be denied emergency medical treatment.”
- Sudan (2005): Commits to free emergency services for all citizens.
Legal provisions alone don’t guarantee effective systems—but they do create a powerful tool for advocacy and accountability. They also recognize that emergency care is not a privilege, but a state responsibility.
The WHO Emergency Care Systems Framework
In 2018, the WHO released a practical tool for assessing and improving emergency care: the Emergency Care Systems Framework. It outlines how emergency care fits within national health systems, and identifies core components for development.
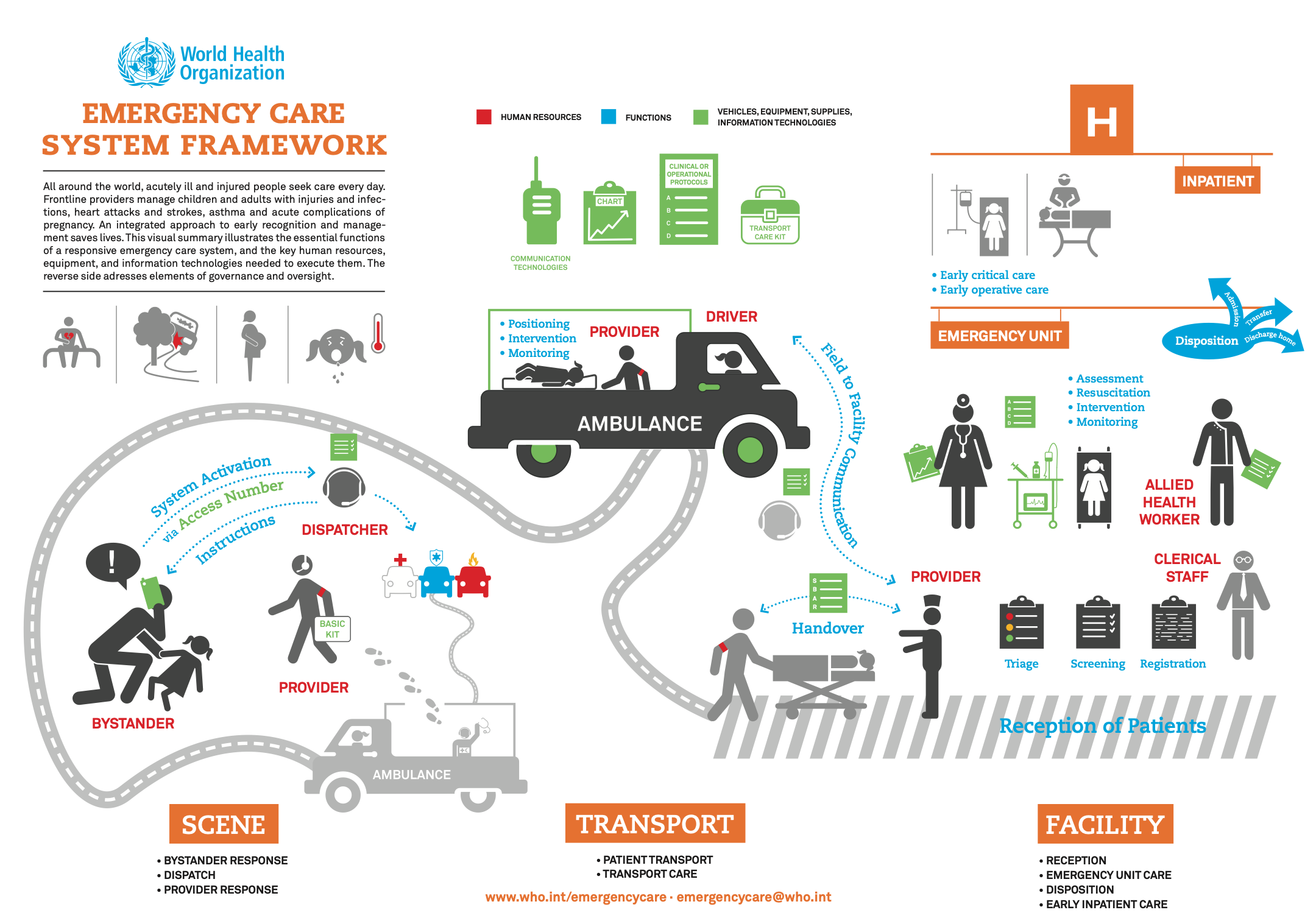
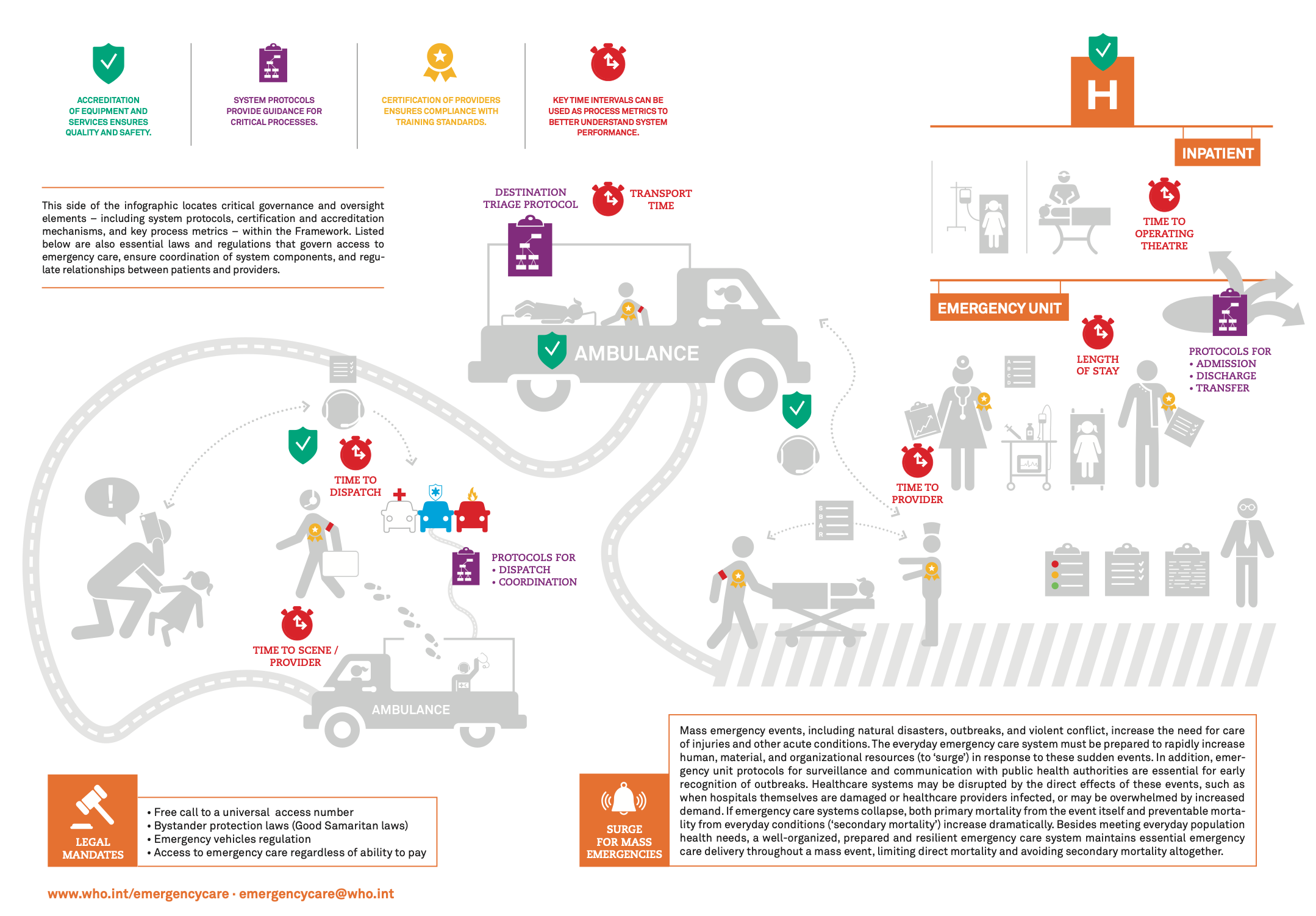
One of the most useful features is the concept of signal functions—minimum services that each level of the system (community, facility, referral centre) should be able to provide. This approach helps countries identify specific gaps and track progress in a standardized way. We can use this framework to structure system assessments, guide quality improvement, or inform advocacy.
Why Does the World Need Emergency Care Systems?
I find existing arguments insufficiently clear or persuasive about why and how we should develop global emergency care systems. My intent is to address this gap critically and transparently, fostering dialogue and informing prioritization.
It is notable that important international work has been done by organizations like the WHO, including developing the Emergency Care System Framework and securing multiple World Health Assembly resolutions. These initiatives have raised awareness and political commitment but it remains unclear their contribution to progress at the national level or disease control priorities.
Foundational Questions to Explore
To build a robust case for emergency care globally, we must clearly answer critical questions and better understand its positioning as a cause priority. Outstanding questions that need answers include:
- What are emergency care-sensitive conditions, and how is their burden globally distributed?
- How does emergency care concretely mitigate the global burden of these conditions?
- Which emergency care-sensitive conditions should receive priority attention within global emergency care initiatives, based on disease control priorities?
- Is improving emergency care a tractable challenge? If so, how do we best approach national-level implementation?
- What is the marginal impact of investments specifically in emergency care compared to other points along the healthcare delivery pathway?
In future posts, I will systematically address these questions through a rigorous application of evidence-based methods, careful reasoning, and comparative analysis.
Concluding Thoughts
Through Critical Good, my goal is to stimulate meaningful dialogue and critical reflection on the impact and effectiveness of emergency medicine. I invite you to join me on this journey, challenging assumptions, rigorously examining evidence, and collectively working toward clearer answers and impactful solutions.